Osteosarcoma
Osteosarcoma is the primary malignancy of bone that occurs in children and adolescents. In contrast to the 93,000 new instances of lung carcinoma and the 88,000 new cases of breast carcinoma that are identified each year, there are around 1,500 new cases of bone sarcoma in the USA. Approximately 20% of primary bone sarcomas are OS, the most prevalent primary solid tumor of bone (Ritter, J., & Bielack, S. S, 2010). The distinguishable by-products of the proliferating cells or their cytologic characteristics serve as the basis for categorization.
The third most common type of bone tumor is called an osteogenic tumor (Messerschmitt, P. J., et al 2009). 1,649 OSs, the most prevalent form of malignant solid bone tumors and the second most common kind of malignant bone tumors overall, were found among the 2,136 osteogenic tumors. In actuality, the growth spurt that occurs during puberty coincides with the peak incidence of OS. The early peak age of females compared to boys, which corresponds to the earlier age of their development spurt, is another piece of evidence in favour of this association (Ottaviani G., 2010).
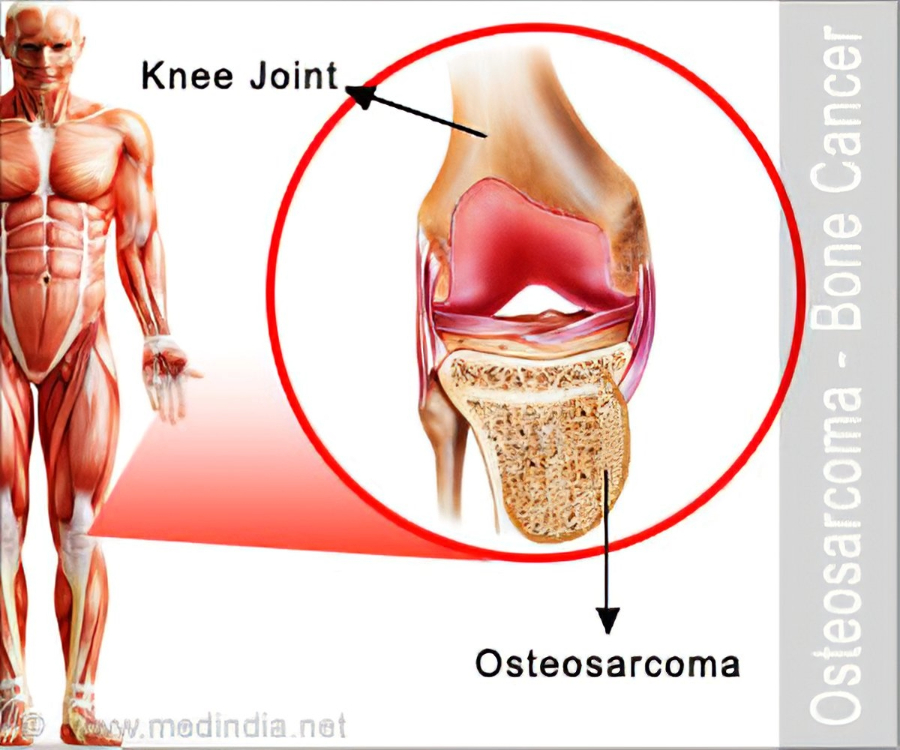
At present, WHO recognizes three major histologic subtypes of OS based on the predominant type of matrix: osteoblastic, fibroblastic, and chondroblastic,(osteoid, fibrous, or chondroid matrix) shown in Figure1(Gorlick R., 2010). Although OS may develop in different kinds of bone, it usually does so in regions where the bone is developing or changing quickly, such as in an adolescent’s long bones. Out of 1,649 instances overall at Mayo Clinic up until the end of 1993, 670 and 303, respectively, were localizations in the distal femur and proximal tibia area. These locations have large growth plates with a high rate of bone turnover and proliferation. With 155 instances within the same period, the proximal humerus is the next prevalent location. The 5-year survival rate for OS in the proximal tibia is 77.5%, marginally higher than that of the distal femur (66%).
Tumor size is one of the most important indicators of prognosis in OS. The most current technique to assess tumor size is absolute tumor volume (ATV), which is determined using a particular ellipsoid formula based on absolute length, depth, and breadth. Based on the aggressive grade, extensive, and distributed levels of OS, staging is carried out. Tumor stages have been categorized by tumor grade (I, low grade; II, high grade), tumor extension (A, intraosseous involvement; B, extraoesseous extension), and the existence of distant metastases (III), by the Musculoskeletal Tumor Society Staging System and Enneking System (Moore, D. D., & Luu, H. H., 2014).
Usually, OS spreads to additional bones or the lungs. Metastasis to other bones can be confined and delayed, indicating the development of a new tumor, or it can be early and extensive, indicating a multifocal origin of the sarcoma (Meyers, P. A., & Gorlick, R., 2010). About 20% of individuals with typical OS had metastases at the time of diagnosis, with 80% of instances being limited to one bone location. The most typical metastatic location is the lung, which is followed by the bone. Usually, lung metastases precede the establishment of bone metastases. “Skip lesions” are tumor nodules that spread over the adjacent joint or inside the same bone but are not within the reactive zone. Metastatic illnesses, most usually affecting the lungs, claimed the lives of 80% of the patients (Lin PP et al., 2012). When pulmonary metastases are discovered at the time of diagnosis, they are typically linked with a poor prognosis.
Chemotherapy doses must be large to influence prognosis, but they also come with serious side effects (Eaton BR et al., 2021). Although some individuals have been helped by radiation therapy and subsequent treatment, the majority of these tumors are not extremely radiosensitive. Therefore, as far as current understanding allows, drastic surgery remains essential (Lindsey BA., 2017). Newer, more potent medications are needed for OS patients, particularly for those who have metastasized or had a relapse of the illness (Beird HC et al., 2022). Preclinical and clinical trials have tested novel medications such as monoclonal antibodies, bisphosphonates, interleukin, and interferon, with hopeful outcomes. Numerous molecular mechanisms or indicators of OS formation and progression have been identified, which holds the prospect of novel, efficient therapies.
Source
- Ritter, J., & Bielack, S. S. (2010). Osteosarcoma. Annals of oncology, 21, vii320-vii325.
- Messerschmitt, P. J., Garcia, R. M., Abdul-Karim, F. W., Greenfield, E. M., & Getty, P. J. (2009). Osteosarcoma. JAAOS-Journal of the American Academy of Orthopaedic Surgeons, 17(8), 515-527
- Ottaviani, G., & Jaffe, N. (2010). The epidemiology of osteosarcoma. Pediatric and adolescent osteosarcoma, 3-13
- Gorlick, R., & Khanna, C. (2010). Osteosarcoma. Journal of bone and mineral research, 25(4), 683-691
- Meyers, P. A., & Gorlick, R. (1997). Osteosarcoma. Pediatric Clinics of North America, 44(4), 973-989
- Moore, D. D., & Luu, H. H. (2014). Osteosarcoma. Orthopaedic oncology: primary and metastatic tumors of the skeletal system, 65-92
- Eaton, B. R., Schwarz, R., Vatner, R., Yeh, B., Claude, L., Indelicato, D. J., & Laack, N. (2021). Osteosarcoma. Pediatric blood & cancer, 68, e28352
- Lindsey, B. A., Markel, J. E., & Kleinerman, E. S. (2017). Osteosarcoma overview. Rheumatology and therapy, 4, 25-43
- Beird, H. C., Bielack, S. S., Flanagan, A. M., Gill, J., Heymann, D., Janeway, K. A., … & Gorlick, R. (2022). Osteosarcoma. Nature Reviews Disease Primers, 8(1), 77
- Lin, P. P., & Patel, S. (2012). Osteosarcoma. In Bone sarcoma(pp. 75-97). Boston,