Unveiling the Role of Gut Microbiota in Type 2 Diabetes: The Story of DPP4
Type 2 diabetes (T2D) is a complex metabolic disorder affecting millions worldwide. One emerging area of research is the role of gut microbiota in diabetes management. Recently, researchers have shed light on the role of DPP4(Dipeptidyl peptidase 4 (DPP-4) inhibitors are a group of antihyperglycemic medications used to manage type 2 diabetes mellitus, which is a significant risk factor for coronary disease, heart failure, stroke, and many other cardiovascular conditions), an enzyme critical in glucose metabolism, which is expressed by specific gut bacteria. This blog explores the latest findings and their implications for diabetes management.
The Significance of DPP4
DPP4, or dipeptidyl peptidase-4, is a key enzyme involved in glucose homeostasis. It plays a crucial role in the regulation of incretins, hormones that stimulate insulin secretion. Inhibition of DPP4 is a well-established therapeutic strategy for T2D, as it increases incretin levels, leading to improved glucose control.
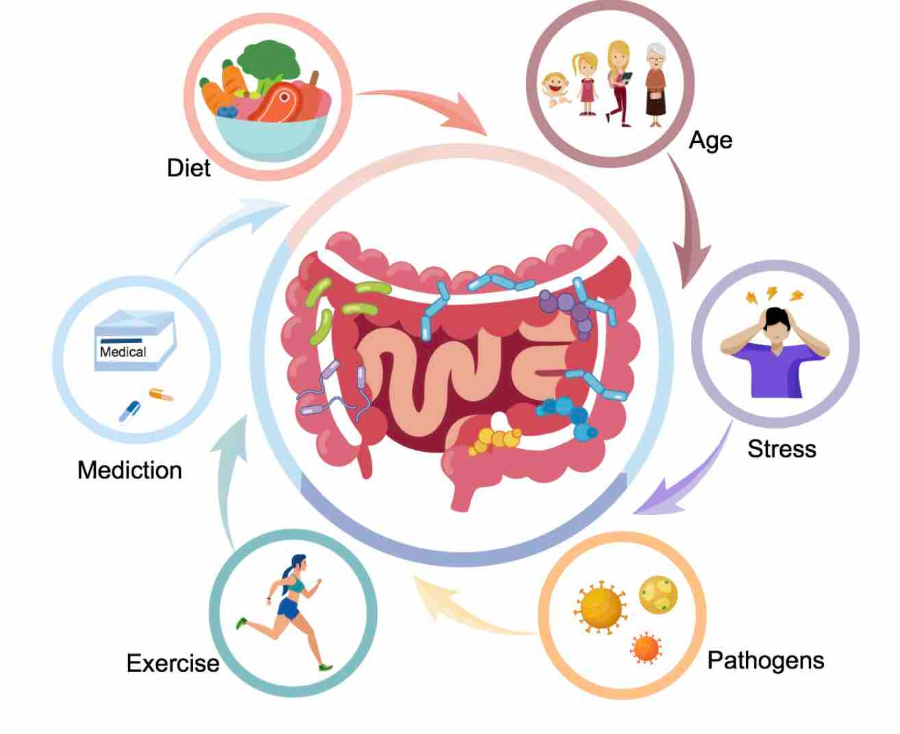
The Gut Microbiota Connection
Recent studies have suggested that gut microbiota may influence DPP4 activity in hosts. However, until now, it was unclear which gut bacteria produce DPP4-like enzymes and what impact this may have on host health. To address this gap, researchers developed a novel platform to investigate microbial-host isozymes. The discovery of microbiota-derived DPP4 opens up new avenues for T2D therapeutics. Modulation of gut microbiota could potentially impact DPP4 activity in hosts, offering a novel approach for managing T2D. Further research is needed to explore the therapeutic potential of targeting gut bacteria to improve glucose metabolism in T2D patients.
The Discovery
Using this platform, researchers identified DPP4 expression in specific Bacteroides species from human and mouse microbiota. This discovery highlights the intricate interplay between gut microbiota and host metabolism. Moreover, it opens new avenues for understanding the role of gut bacteria in T2D.
Studies
Research indicates that two major types of bacteria, Bifidobacterium and Bacteroides, have been consistently associated with Type 2 diabetes (T2D) in numerous studies. These studies have reported an abundance of these genera in individuals with T2D. Additionally, other genera such as Roseburia, Faecalibacterium, and Akkermansia, while not as frequently mentioned as Bifidobacterium and Bacteroides, were also found to be consistently negatively associated with T2D in human studies. These genera are believed to have beneficial effects on metabolism and inflammation, which may contribute to their protective role against T2D. However, more research is needed to fully understand their impact on T2D and whether interventions targeting these genera could be beneficial for T2D management. The associations between specific bacterial genera and T2D highlight the potential of microbiota-targeted interventions for T2D management. Modulating the gut microbiota through diet, probiotics, or other interventions could potentially alter the risk or progression of T2D. However, more research is needed to identify the most effective strategies for targeting the microbiota in the context of T2D.
In consideration of lactobacillus species, The Lactobacillus genus presents a complex case in the context of Type 2 diabetes (T2D), with apparently discordant results in association studies, including those analysing changes after treatments. However, cross-sectional studies comparing patients versus controls have reported a positive association between the abundance of this genus and T2D in five out of six papers. Furthermore, associations of this genus tend to be species-specific. For example, while L. acidophilus, L. gasseri, and L. salivarius were increased in T2D patients, L. amylovorus was decreased, suggesting a high diversity in functional impact on host metabolism by bacteria from this genus.
Several species from the Lactobacillus genus have been tested as probiotics, with experimental studies in mice showing mostly beneficial effects in models of T2D. However, the effects of Lactobacillus species on T2D in human clinical trials have been mixed. Out of eleven studies that showed some protective effect, the majority combined other genera, most frequently Bifidobacterium, suggesting that Lactobacillus and Bifidobacterium may work synergistically. Species like L. sporogenes, L. casei Shirota, and L. reuteri used as mono-probiotics have been reported to improve T2D-related symptoms in humans. L.plantarum, a bacterium found in fermented food products, is intensively studied in animal systems, with many studies showings that it improves glucose metabolism in mice models of T2D. However, clinical trials have not shown significant effects on glucose metabolism. It appears that Lactobacilli’s anti-diabetic effect is seen more frequently when they are part of a probiotic cocktail rather than administered individually.
Overall, the Lactobacillus genus is highly diverse and contains the highest number of operational taxonomic units (OTUs) in the human gut among potentially probiotic bacteria. Its effects on T2D seem to be species-specific or even strain-specific, which might explain why genus-level analysis lacks consistency among studies using these bacteria.
Fewer studies have reported positive associations of microbiota with T2D and/or hyperglycemia. Specifically, Ruminococcus, Fusobacterium, and Blautia have been reported in a positive association with T2D.
Implications for Diabetes Management
The discovery of microbiota-derived DPP4 has significant implications for T2D management. It suggests that modulation of gut microbiota could potentially impact DPP4 activity in hosts, offering a novel therapeutic approach. Further research is needed to explore the therapeutic potential of targeting gut bacteria to improve glucose metabolism in T2D patients.
The discovery of DPP4 expression by specific gut bacteria unveils a new chapter in our understanding of the role of gut microbiota in T2D. while some bacterial taxa have been systematically implicated in T2D, overall diversity and other macro-metrics of microbial communities have not shown a consistent relation to diabetes. Some taxa, such as Bacteroides and Bifidobacterium, are consistently associated with protection from T2D, while others, like Lactobacilli, show only species- or strain-specific effects. Importantly, several of these microbes are currently being tested as probiotics in mouse and human studies. It highlights the potential of targeting microbiota-derived DPP4 as a novel therapeutic strategy for diabetes management. Future research in this area promises to revolutionize T2D treatment and improve the lives of millions affected by this disease.
Source